For a long time, this implant has allowed him to control computers and prosthetic limbs using only his mind.
Nathan Copeland sometimes thinks of himself as a robot.
This 36-year-old man has lived with a brain-computer interface for more than seven years and three months, as of August 17, 2022. This is also the longest time a human has possessed such an implant. It consists of a grid of electrodes the size of a pencil eraser, surgically implanted into Copeland’s motor cortex, converting nerve impulses into commands that allow him to control external devices such as computers, video games, and robotic arms just by thinking.
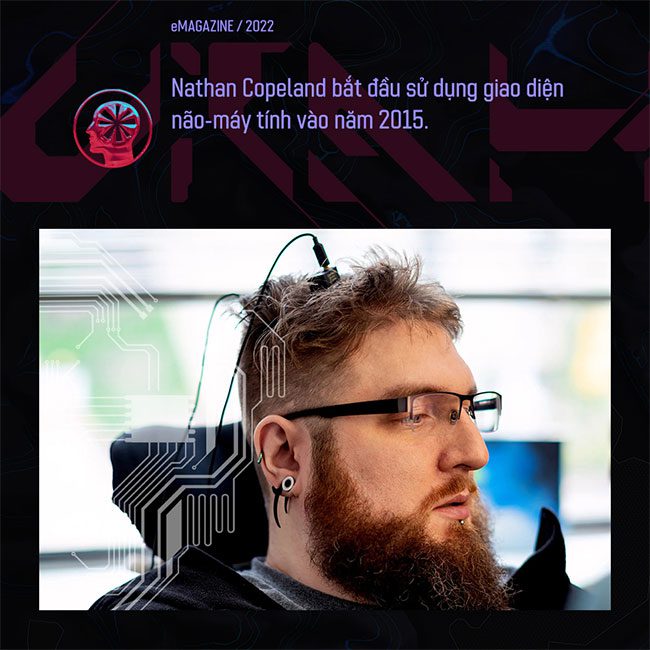
Looking back, a car accident in 2004 left Copeland paralyzed from the chest down, unable to move or feel his limbs. In 2014, he participated in a study at the University of Pittsburgh for individuals with spinal cord injuries to see if a brain-computer interface (BCI) could restore some of the functions he had lost. He did not hesitate to enroll, even though it would require brain surgery, and at that time, no one knew how long the device would last.
“When I started, they said, ‘Oh, it might last 5 years.’ In reality, that number was based on data from monkeys, because no human had done it before,” he said.

Copeland’s implant is still functioning—and has not caused any significant side effects or complications—offering hope for this field. It is a sign that these devices, which have been in development since the 1960s but are still experimental, are getting closer to commercial deployment for severely disabled patients. Jane Huggins, director of the Brain Interface Laboratory at the University of Michigan, who is not affiliated with the Pittsburgh study, stated: “It seems to be on the verge of entering reality.”
However, questions remain, primarily about the long-term durability of the implanted arrays. No one knows how their performance will degrade over time and whether they can be upgraded. “It would be crazy to regain function for many years, only to lose it again. And that’s always a concern with implants when used as a service requirement,” Huggins said.
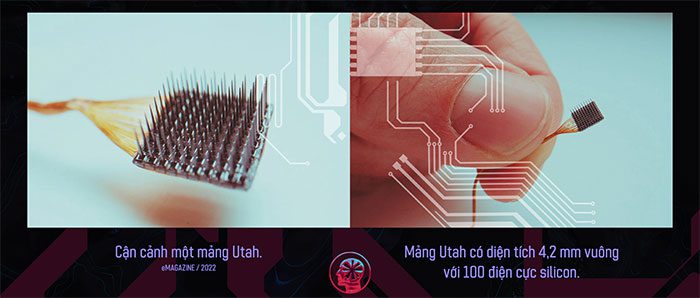
Copeland received his first array in 2015 and subsequently received three more as part of the study, giving him a total of four active implants. Known as the Utah array, they are made of hard silicon and resemble the bristles of a hairbrush. A standard array is a square grid with 100 tiny needles, each about one millimeter long and coated with a conductive metal. Since neurons generate electric fields when they communicate, scientists can use these arrays to capture and record activity from hundreds of nearby neurons.
To build the brain-computer interface, researchers must translate those neural signals into digital commands that allow the user to control prosthetic limbs or computers. The system Copeland uses, known as BrainGate, consists of an implanted array, a cable running from a small battery-sized pad on his head to an external device that amplifies his neural signals, and a computer running software to decode those signals.
Richard Normann, a professor of biomedical engineering at the University of Utah, was the first to shape the Utah array in the 1980s while trying to restore vision. Since then, it has become the gold standard for brain-computer interface research.
“The entire field is built on the Utah array,” said Matt Angle, CEO of Paradromics, a Texas-based BCI company. “The fact that we have been relying on a device designed in the 80s and 90s shows how ahead of its time it was.”
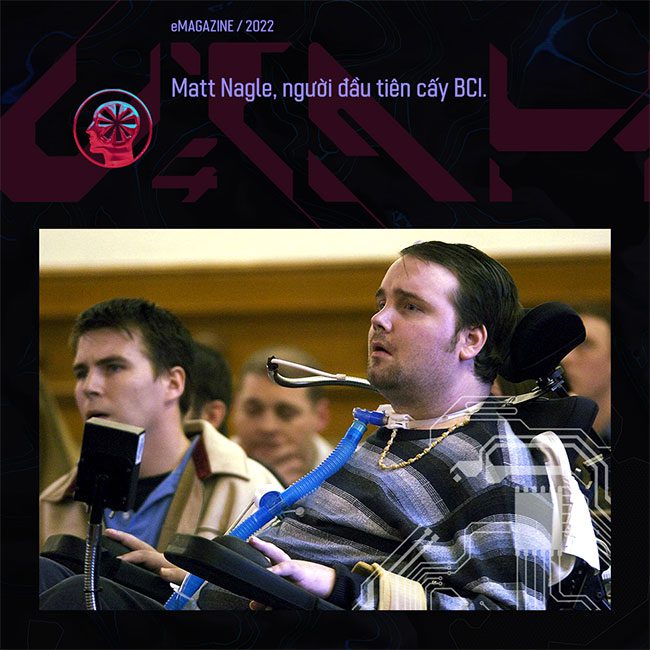
In 2004, Matt Nagle became the first paralyzed person to receive a Utah array implant. It allowed him to move a computer cursor, operate a TV, check emails, and open and close a prosthetic hand. Nagle’s implant was removed after one year, as part of the study he participated in. Currently, there are over 30 participants in studies worldwide wearing implanted BCIs. Ian Burkhart was previously the record holder for the longest-lasting BCI implant until he removed it in 2021 when the related study concluded.
With very few people equipped with these devices, their longevity remains uncertain. So far, the Utah array has operated for up to 10 years in monkeys. In Copeland’s case, his arrays are still functioning, but not as well as in the first year after implantation, according to Robert Gaunt, a biomedical engineer at the University of Pittsburgh and a member of Copeland’s research team.
“The body is a very difficult place to implant electronics and systems,” Gaunt said. “It’s an aggressive environment, and the body is always trying to eliminate these things.”
The implanted arrays can trigger immune responses in the neural tissue surrounding the electrodes, which are the sharp probes that attach to the brain. Studies have shown that this inflammation can lead to reduced signal quality. Additionally, scar tissue can form around brain implants, which also affects the ability to receive signals from nearby neurons. The less information the BCI can interpret from the neurons, the less effective it is at performing intended functions.
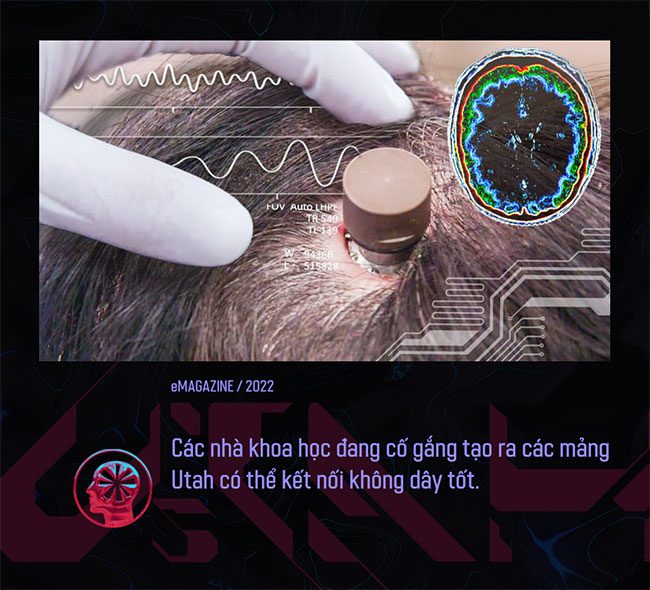
One way scientists are trying to make implants last longer is by experimenting with different materials. The Utah array is insulated with parylene, a protective polymer coating used in medical devices for its stability and low moisture absorption. However, it can corrode and crack over time, and other materials may prove to be more durable.
Florian Solzbacher, co-founder and president of Blackrock Neurotech, the company that manufactures the Utah array, stated that the company is testing a material coated with a combination of parylene and silicon carbide. He said, “We have seen their lifespan could be up to 30 years, and we have some preliminary data in animals. But the company has not yet implanted it in humans, so the real test will be how human tissue reacts to the new material formulation.”
Making the electrodes more flexible could also be a solution to reduce scarring. Angle’s company, Paradromics, is developing an implant similar to the Utah array but with thinner electrodes intended to cause less disruption to the tissue.
Some researchers are testing softer materials so they can integrate better into the brain compared to the rigid Utah arrays. A team at the Massachusetts Institute of Technology is experimenting with hydrogel coatings designed to have elasticity very similar to that of the brain. Scientists at the University of Pennsylvania are also developing “living” electrodes, with tiny hair-like fibers made from neurons and nerve fibers grown from stem cells.
However, these approaches also have downsides. “You can turn something rigid into something soft. But if you’re trying to put something very soft into something else that is also soft, that can be very challenging,” Gaunt said.
Another approach is to make the implants smaller, thus reducing invasiveness. For example, researchers are experimenting with neuron particles, tiny chips the size of a grain of sand, which could potentially be scattered across the surface of the cortex. However, no one has yet tried to disperse them on human brains, and this system has only been tested on rodents with their skulls removed.
Some study participants have had their Utah arrays removed and replaced, but undergoing multiple surgeries is not ideal. Each surgery carries risks of infection or bleeding at the implant site. Gaunt stated that surgeons would likely not place a new implant in the same position as an old one, especially if there is scarring in that area. But ensuring that the replacement is positioned correctly is also a concern, as misplacing the implant can lead to cognitive and communication impairments.
Gaunt suggested it would be better if the external BCI components—such as processors or software—could be upgraded, so patients do not have to undergo multiple surgeries.
However, in reality, an external part of most new Brain-Computer Interface (BCI) systems poses one of the biggest risks associated with brain implants. Although the mounts placed on top of the skull tend to cause infections, their presence is necessary to connect the implanted array to an external computer. Currently, Nathan Copeland and other research participants have to plug wires into the system through a head mount to use their BCIs. Researchers are working to eliminate these cables.
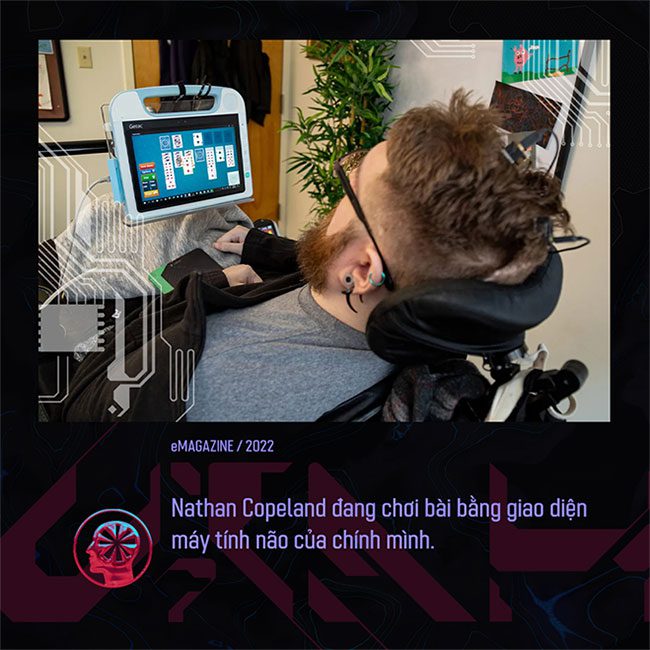
For Copeland, it is a minor inconvenience in exchange for the things he can do with his BCI. Nonetheless, he hopes that future systems will be wireless and provide those with paralysis a broader range of movement or capabilities.
With uncertainties regarding the longevity of BCIs, Copeland knows that his implant may eventually stop working. However, he is trying not to worry about that and would not refuse an upgrade. “In 5 or 10 years, if there is something that can significantly improve, I would have the surgery again and keep moving forward,” he stated.



















































